- Visibility 22 Views
- Downloads 3 Downloads
- DOI 10.18231/j.sajhp.2024.023
-
CrossMark
- Citation
Examining the relationship between medical doctors' lifestyle behaviors and the incidence of lifestyle-related diseases: An observational cohort study
- Author Details:
-
Ajay M Godse *
-
Nayana B Gosavi
-
Bhagyashri L Karande
-
Vaidehi A Nawathe
Introduction
Healthy habits among physicians are crucial for guiding patients towards preventing chronic diseases. General practitioners (GPs) serve as health role models and are more inclined to advise patients on lifestyle behavior change if the GP themselves follow healthy habits. Practicing what they preach is a significant factor influencing physicians' ability to counsel patients effectively on health promotion.[1] Currently, a “healthy lifestyle” is defined as engaging in sufficient physical activity, having a well-balanced diet, a Body Mass Index (BMI) within the recommended range, a non or moderate consumption of alcohol, being a non-smoker and obtaining sufficient daily sleep.[2] Despite the established criteria for a "healthy lifestyle," a study in the southern region of India revealed that among 240 doctors surveyed, 54% (114) were overweight or obese. Additionally, 54.5% of doctors reported low levels of physical activity.[3] Doctors and nurses play a pivotal role in ensuring the well-being of patients by delivering essential healthcare services. It's crucial for health care workers to prioritize their own health. Yet, due to the nature of their work, many doctors and nurses lead predominantly sedentary lifestyles, which can inadvertently place them at higher risk for cardiovascular diseases (CVDs) when preventive health measures aren't consistently followed by them. A longitudinal study spanning two decades in Brazil examined various healthcare professionals, revealing concerning trends such as notable weight gain and a notable rise in the occurrence of systemic arterial hypertension and also reported an increased prevalence of dyslipidemia and excessive alcohol consumption among doctors and nurses. These findings signify the importance of promoting healthier habits within the healthcare community to safeguard their wellbeing.[4] Another study carried out in Singapore to estimate the prevalence of cardiovascular risk factors among health workers (doctors and nurses) reported that around 10% of the doctors and nurses were having dyslipidemia, and around 7% of them were obese (body mass index >30 kg/m2). [5] India is one among the epicenters of Diabetes Mellitus (DM) pandemic worldwide. The sharp rise in the prevalence of DM in India has likely been caused by quick demographic shift and socioeconomic advancement.[6], [7] The results from a study concluded that 29.7% of the medical doctors who were assessed had an increased 10 year risk of type 2 diabetes mellitus [34]. According to a study conducted in Tamil Nadu India, reported prevalence of Diabetes mellitus (25.4%),Hypertension(29.4%), overweight (36.5%) ,obesity (15.1%).[8]
According to several recent study, hours of sleep among physicians averaged between 5.9 h and 6.5 h of daily sleep.[9] Insufficient sleep proved to be associated with decreased performance, increased stress and burnout, and higher risk of obesity, diabetes and hypertension.[10] There is research that risky behaviours such as consuming alcohol, using tobacco, and eating unhealthy have a correlation and frequently occur together or in groups in most of the physicians.[11] The World Health Organisation (WHO) recommends that people should engage in doing moderate to intense exercise for 150 minutes of or at least strenuous exercise for 75 minutes of per week.[12] However, evidence points to a low Physical Activity (PA) level among physicians. In Cameroon, primary healthcare providers (PHCPs) participated in a study that revealed 86% of them did not maintain the necessary physical activity level.[13] Similarly, a cross-sectional survey conducted in Bahrain revealed that only 29.6% of doctors exercised for at least 30 minutes per week, and only 13% reported physical activity for at least five days per week.[14] Even with the increasing positive evidence regarding the benefits of physical activity (PA) and the consensus among healthcare professionals (HCPs) on the importance of promoting PA to patients, studies reveal that numerous physicians do not actively engage in such promotion , moreover, despite the crucial nature of this matter, few studies have investigated the health-promoting lifestyle profile (HPLP) among medical doctors.[15]
Assessing the presence of health-related lifestyle factors among physicians is essential, as healthy behaviors may not only significantly reduce mortality and morbidity but will also have a notable impact on counselling of their patients In order to determine whether medical doctors who themselves counsel patients to lead healthy lifestyles also adhere to that advice in their daily lives, this study was conducted with an objective to assess the lifestyle behaviours of medical doctors (consultants, non-clinical physicians, resident medical assistants, and post-graduate medical students) of tertiary care centers with a view of investigating this topic and educating doctors about health promoting behavior and practices.
Methods and Materials
This was a prospective, observational, single center study conducted from April 2023 to June 2023 at the department of Pulmonology and Sleep Medicine of Bhaktivedanta Hospital and Research Institute, Thane, India. This study was approved by the Institutional Ethics Committee (IEC) and has been registered with CTRI (CTRI/2023/03/051184). Considering the confidence level of 95% and relative precision of 307.56, a total sample size of 146 doctors were calculated.
The study started post obtaining non-objection certification by Director of the institute. All the doctors of the institute were briefly explained about the objective of the study, and consequently a questionnaire through google form were circulated online which had additionally a consent form incorporating the details of purpose of the study and a permission to use their respective data in the study. The form was designed with questions regarding their demographic details, details of comorbid conditions, family history of comorbid condition, duration and nature of physical activity, their dietary habits, sleep habits, smoking habits and questions regarding alcohol use were also asked, the questionnaire was well validated and approved by EC. Out of all doctors, a total of 74 doctors filled the questionnaire, for whom physical assessments were conducted within 20 days of filling of the questionnaires, the physical assessment involved evaluation of height, weight, BMI, SpO2 (%), BP, body fat, subcutaneous fat, visceral fat. Measurements of circumference of neck, waist, and hip.
The numeric data were summarized by descriptive statistics like n, mean ± SD, median, minimum, and maximum. Before applying any statistical test, a normality test was performed. The categorical data were summarized by frequency count, and percentage and significance were analyzed using the chi-square test. All statistical data was analyzed by IBM SPSS software v.23.0. A p-value less than 0.05 was considered statistically significant.
Results
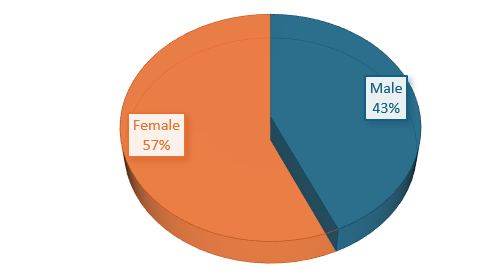
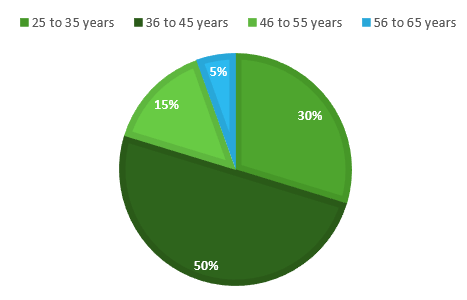
In our study out of 74 physicians, 32 (43%) individuals were male, while 42 (57%) were female, with most common age group being 36 to 45 years (50%) 25 to 35 years (30%), 46 to 55 years (15%), and 56 to 65 years (5%) ([Figure 1], [Figure 2])
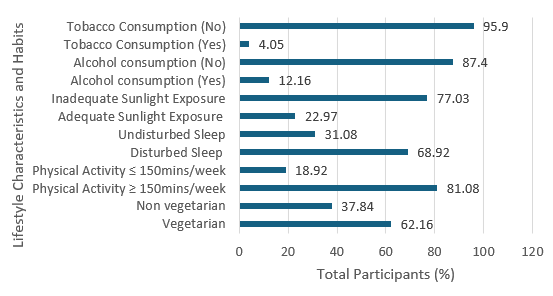
In terms of dietary habits, 46 (62.16%) were vegetarian, whereas 28 (37.84%) were non-vegetarian. Regarding physical activity (PA) levels, 60 (81.08%) participants of the sample, engaged in ≥ 150 minutes of PA per week, while 14 (18.92%) participants, reported engaging in ≤ 150 minutes of PA per week ([Figure 3]). However, no significant association was observed between physical activity and visceral fat (p-value = 0.38), nor between physical activity and body fat composition (p-value = 0.57) ([Table 1]).
Sleep patterns were categorized as disturbed, in 51 (68.92%) participants, and undisturbed, in 23 (31.08%) participants. In our study, 17 individuals (22.97%) received sufficient sunlight exposure, while 57 individuals (77.03%) did not receive adequate sunlight exposure. Additionally, alcohol consumption was reported by 9 (12.16%) participants, and tobacco consumption was reported by 3 (4.05%) participants ([Figure 3]).
The present study did not find any statistically significant correlation between diet and visceral fat (p- value = 0.583), nor between diet and body fat composition (p-value = 0.499). Similarly, our analysis revealed no significant association between sleep and visceral fat (p-value = 0.77), as well as between sleep and body fat (p-value = 0.674) ([Table 1])
The correlation between visceral fat and BMI across different diet groups was observed. For participants following a vegetarian diet, the correlation coefficient (r value) is reported at 0.539 with a corresponding p-value of less than 0.0001, indicating a significant correlation. Conversely, in the non-vegetarian diet group, the correlation coefficient stands at 0.564, with a p-value of 0.002, also indicating a significant correlation. These findings suggest that both vegetarian and non-vegetarian dietary patterns exhibit notable correlations between visceral fat levels and BMI, highlighting the importance of diet in relation to body composition and health outcomes. ([Table 2])
|
Variables |
Value |
df |
Asymptotic Significance (2-sided) |
Exact Sig. (1-sided) |
|
Corelation between Diet and Visceral Fat Association |
|
|
|
|
|
Pearson Chi-Square |
.005a |
1 |
.943 |
|
|
Continuity Correctionb |
.000 |
1 |
1.000 |
|
|
Likelihood Ratio |
.005 |
1 |
.943 |
|
|
Fisher's Exact Test |
|
|
|
.583 |
|
Corelation between Diet and Body Fat Association |
|
|
|
|
|
Pearson Chi-Square |
.330a |
1 |
.566 |
|
|
Continuity Correction b |
.000 |
1 |
1.000 |
|
|
Likelihood Ratio |
.293 |
1 |
.589 |
|
|
Fisher's Exact Test |
|
|
|
.499 |
|
Corelation between physical activity and Visceral Fat Association |
|
|
|
|
|
Pearson Chi-Square |
.342a |
1 |
.559 |
.383 |
|
Continuity Correction b |
.095 |
1 |
.758 |
|
|
Likelihood Ratio |
.347 |
1 |
.556 |
.383 |
|
Fisher's Exact Test |
|
|
|
.383 |
|
Corelation between physical activity and body Fat Association |
|
|
|
|
|
Pearson Chi-Square |
.138a |
1 |
.710 |
.572 |
|
Continuity Correction b |
.000 |
1 |
1.000 |
|
|
Likelihood Ratio |
.129 |
1 |
.720 |
.572 |
|
Fisher's Exact Test |
|
|
|
.572 |
|
Corelation between sleep and Visceral Fat Association |
|
|
|
|
|
Pearson Chi-Square |
3.246a |
1 |
.072 |
.077 |
|
Continuity Correction b |
2.066 |
1 |
.151 |
|
|
Likelihood Ratio |
3.168 |
1 |
.075 |
.077 |
|
Fisher's Exact Test |
|
|
|
.077 |
|
Corelation between sleep and Body Fat Association |
|
|
|
|
|
Pearson Chi-Square |
.433a |
1 |
.511 |
.674 |
|
Continuity Correction b |
.000 |
1 |
1.000 |
|
|
Likelihood Ratio |
.795 |
1 |
.372 |
.674 |
|
Fisher's Exact Test |
|
|
|
.674 |
|
Groups |
Parameters |
|
|
Vegetarian diet group |
r Value |
P Value |
|
0.539 |
<0.0001 |
|
|
Non-vegetarian diet group |
0.564 |
0.002 |
Discussion
The demanding nature of medical work can also take a toll on doctors' physical health.[16] According to a recent study conducted in India to evaluate the prevalence of metabolic syndrome in physicians, it was observed that there were significantly higher metabolic syndrome rates among females than in males.[17] The results of the present study shows a lower prevalence of hypertension (12.1%), diabetes (5.4%) among physicians However, a study carried out on the lifestyle habits and well-being of physicians in middle-east India in 2015 reported a higher prevalence of hypertension (20.3%) and diabetes (11%). [18] One possible reason for the increased prevalence of lifestyle disorders among doctors could be the demanding nature of their profession, which often leads to irregular working hours, high stress levels, and limited time for self-care activities such as exercise and healthy eating which can contribute to increased risks of obesity, cardiovascular disease, and other health problems.[19]
Research on physicians' BMI, which indicated that around one-third of every 10 physicians were either overweight or obese.[19] In our study, a significant negative correlation was obtained between physical activity and Body fat association and visceral fat ([Table 1]). In our study, 31 (41.8%) physicians were overweight whereas 14 (8.9%) physicians were obese which aligns to a study done on predictors of obesity among postgraduate trainee doctors, which observed that the prevalence of overweight was 31.6% and obesity was 28.2%.[20] The results of the current study also aligns with a study conducted among doctors at the University of Brunei Darussalam, in which the prevalence of overweight and obesity was found to be 37% and 17%, respectively. [19] Additionally, patients of overweight and obese doctors are less likely to follow their doctors' medical recommendations than patients of doctors who are of a healthy weight.[21]
A study carried out about dietary habits among health-care professionals in Saudi Arabia reported a high percentage of participants who regularly ate dairy foods (74%), meat (91%), and sweet foods (60%) and drank carbonated beverages with sugar (55%) and alcohol (65%). Most participants rarely ate fruits (77%) and vegetables (73%).[22] In another survey carried out on the dietary habits of medical students, states that only 13 participants (10%) had fruit consumption.[21] The results of this studies were inconsistent with our findings wherein 41 (55%) have 1 to 6 teaspoon refined sugar whereas 33 (44.5%) have no sugar consumption in their daily life. Whereas only 31.8% participant had soft drinks and beverages in their daily lives. 24.3% eat red meat once in a week and most of the participants were 62.16% were vegetarian ([Figure 3]) with their diet consisting of vegetables, fruits, whole grains.
In our study there is a significant correlation between visceral fat and BMI with vegetarian diet group participants (p value =<0.0001) ([Table 2]), which is in similar lines with other cross-sectional studies which also observed a significantly greater reduction in visceral fat and BMI in individuals consuming plant-based diets.[23], [24] The survey involved an intervention with a low-fat vegetable-based diet and vegetable meal replacement (intervention group) and an omnivorous diet. The authors observed significant reduction in weight, body fat, and visceral fat in interventional group.[25] Our study found a significant correlation between visceral fat and BMI in non-vegetarian group participants (p value = 0.002) ([Table 2]). The results are in similar lines with studies that found statistically significant differences in body composition and BMI in participants who have vegetable-based and omnivorous diets combined.[26]
We found that the medical doctors of our tertiary care hospital were sleeping for a lesser time per night (6.3 [6.0-6.7] hours) than the 7 hours or more, recommended by the American Academy of Sleep Medicine and Sleep Research Society.[27] In our study 68.92% of physicians had disturbed sleep ([Figure 3]). The excessive workload compounded by the inadequate sleep in them can be a threat to the health of both the physician and the patient. Prolonged sleep restriction has been reported to reduce the cognitive and clinical performance of physicians, Further, sleep-deprived doctors are vulnerable to the well-described long-term consequences of chronic sleep loss that include obesity, type II diabetes mellitus, and increased cardiovascular diseases. However, in our study we found no statistically significant association between sleep and body fat and visceral fat ([Table 2]).
The limitation of the current study, is its study design which is single centric conducted at a tertiary care centre. A multi-centric study with a larger sample size catering to a heterogenous population could have been more reliable. The questionnaire used in the study is elaborate which could be a reason for recall bias by the physicians given the time constraint.
Conclusion
It's crucial for doctors to intrinsically motivate themselves to adopt healthy lifestyles, not only for their own professional well-being but also as advocates for promoting overall physical and psychological health within society.
Our findings align with numerous other studies, emphasizing the necessity for a carefully devised strategy to address financial and technological barriers hindering the accurate identification of health risk factors and the implementation of corrective interventions.
It is imperative to integrate healthy dietary habits and regular exercise into daily routines. Notably, half of the doctors reported experiencing insomnia due to their extensive professional commitments. Certain dietary patterns, levels of physical activity, and lifestyle choices appear to correlate with the demanding schedules and prolonged working hours commonly experienced in the medical profession.
Source of Funding
None.
Conflict of Interest
None.
References
- SM Ahmed, A Hadi, A Razzaque, A Ashraf, S Juvekar, N Ng. Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants. . Glob Health Action 1986. [Google Scholar]
- W Miron, R Malatskey, L Rosen. Health-related behaviours and perceptions among physicians: results from a cross-sectional study in Israel. BMJ Open 2019. [Google Scholar]
- A Nair, T Lawrence, P Indu. Obesity burden and physical activity pattern among doctors in South India. Indian J Occup Environ Med 2022. [Google Scholar]
- TV Jardim, A Sousa, TR Povoa, WS Barroso, B Chinem, PCV Jardim. Comparison of Cardiovascular Risk Factors in Different Areas of Health Care Over a 20-Year Period. Arquivos Brasileiros de Cardiologia 2014. [Google Scholar]
- L Leong. Prevalence of cardiovascular risk factors among healthcare staff in a large healthcare institution in Singapore. Singapore Med J 2012. [Google Scholar]
- R Unnikrishnan, RM Anjana, V Mohan. Diabetes mellitus and its complications in India. Nat Rev Endocrinol 2016. [Google Scholar]
- R Unnikrishnan, R Pradeepa, SR Joshi, V Mohan. Type 2 Diabetes: Demystifying the Global Epidemic. Diab 2017. [Google Scholar]
- SKB Hegde, S Sathiyanarayanan, S Venkateshwaran. Prevalence of Diabetes, Hypertension and Obesity among Doctors and Nurses in a Medical College Hospital in Tamil Nadu. India Nat J Res Commun Med 2015. [Google Scholar]
- Y Wu, F Jiang, S Wu, Y Liu, YL Tang. Sleep duration and satisfaction among physicians in tertiary public hospitals in China: a large sample national survey. J Occup Med Toxicol 2021. [Google Scholar]
- HR Colten, BM Altevogt. . Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorder 2006. [Google Scholar]
- AA Mohd, A Lai, H Parveen, SK Ong. Prevalence of overweight and obesity among doctors in Brunei Darussalam. Brunei Int Med J 2016. [Google Scholar]
- . World Health Organization. Physical activity. www.who.int.. 2023. [Google Scholar]
- M Alyafei, M Alchawa, A Farooq, N Selim, I Bougmiza. Physical Activity among Primary Health Care Physicians and Its Impact on Counseling Practices. Biomed Hub 2023. [Google Scholar]
- SM Borgan, GA Jassim, ZA Marhoon, MH Ibrahim. The lifestyle habits and wellbeing of physicians in Bahrain: a cross-sectional study. BMC Public Health 2015. [Google Scholar]
- FA Albert, MJ Crowe, A Malau-Aduli, M Aduli Bs. Physical Activity Promotion: A Systematic Review of The Perceptions of Healthcare Professionals. Int J Environ Res Public Health 2020. [Google Scholar]
- A Koinis, V Giannou, V Drantaki, S Angelaina, E Stratou, M Saridi. The Impact of Healthcare Workers Job Environment on Their mental-emotional health. Coping strategies: the Case of a Local General Hospital. Health Psychology Research. Health Psychol Res 2015. [Google Scholar]
- DS Prasad, Z Kabir, AK Dash, BC Das. Prevalence and risk factors for metabolic syndrome in Asian Indians: A community study from urban Eastern India. J Cardiovascular Dis Res 2012. [Google Scholar]
- R Garg, P Agrawal, AP Singh, M Agrawal, P Gupta. Glimpse into the Lifestyle of Doctors. J Mid-Life Health 2022. [Google Scholar]
- S Mahmood, R Najjad, N Ali. Predictors of obesity among post graduate trainee doctors working in a tertiary care hospital of public sector in Karachi. J Pak Med Assoc 2010. [Google Scholar]
- SH Kunene, NP Taukobong. Dietary habits among health professionals working in a district hospital. Afr J Pri Health Care Fam Med 2017. [Google Scholar]
- AM Pinto, T Sanders, AC Kendall, A Nicolaou, R Gray, H Al-Khatib. A comparison of heart rate variability, n-3 PUFA status and lipid mediator profile in age- and BMI-matched middle-aged vegans and omnivores. Brit J Nutr 2017. [Google Scholar]
- N Vibhute, R Baad, U Belgaumi, V Kadashetti, S Bommanavar, W Kamate. Dietary habits amongst medical students: An institution-based study. Journal of Family Medicine and Primary Care 2018. [Google Scholar]
- F Sofi, M Dinu, G Pagliai, F Cesari, A M Gori, A Sereni. Low-Calorie Vegetarian Versus Mediterranean Diets for Reducing Body Weight and Improving Cardiovascular Risk Profile: CARDIVEG Study (Cardiovascular Prevention With Vegetarian Diet). Circulation 2018. [Google Scholar]
- A Brytek-Matera. Interaction between Vegetarian Versus Omnivorous Diet and Unhealthy Eating Patterns (Orthorexia Nervosa, Cognitive Restraint) and Body Mass Index in Adults. Nutrients 2020. [Google Scholar]
- L Shaik, MS Cheema, S Subramanian, R Kashyap, SR Surani. Sleep and Safety among Healthcare Workers: The Effect of Obstructive Sleep Apnea and Sleep Deprivation on Safety. Medicina (Kaunas) 2022. [Google Scholar]
- A Priya, E Tharion. Sleep and Exercise among Young Doctors in a Tertiary Care Hospital in India: A Pilot Cross-Sectional Study. J Lifestyle Med 2022. [Google Scholar]
- L Shaik, M S Cheema, S Subramanian, R Kashyap, S R Surani. . Sleep and Safety among Healthcare Workers: The Effect of Obstructive Sleep Apnea and Sleep Deprivation on Safety 2022. [Google Scholar]
