- Visibility 485 Views
- Downloads 35 Downloads
- DOI 10.18231/j.sajhp.2024.009
-
CrossMark
- Citation
Importance of case history in disease diagnosis as perceived by medicos
Introduction
The focus of training in undergraduate medicine is to make the student a good diagnostician of all the simple illnesses which make up most of the health problems in any community. The tools available for the medical student to make a reasonable working diagnosis are history taking followed by clinical examination. As an implement for diagnosis, history taking is considered the most powerful, sensitive and most versatile instrument available to the physician.[1] A medical history of a patient comprises an extensive inquiry into all the medical issues surrounding him / her and all previous interactions and experiences with the medical world.[2]
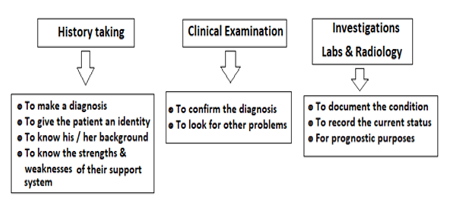
The role of investigations as a first line diagnostic tool for an undergraduate doctor is debatable. Investigations at this level are more useful for documenting the disease condition and prognostic purposes. History taking or the medical interview calls for interpersonal and patient interview skills and is an essential skill that must be taught in the course of medical education. The medical interview not only helps the patient to recall information but also aids in diagnostic accuracy, patient and physician satisfaction, patient adjustment to stress and illness, adherence to therapy and health outcomes.[3]
Diagnosis drives therapeutic decisions and even in this hi-tech age, the very human process of clinical reasoning leads to accurate diagnosis and to high quality safe patient care.[4] The process of clinical reasoning helps give a comprehensive view of the patient’s needs and aids in patient centered care. This process includes mainly history taking and physical examinations and also a review of laboratory data thereby determining a final diagnosis.[5] Previous research has shown that physicians make diagnoses from the patients’ history alone in almost 90 percent of cases.[6], [7]
Considering the correct diagnosis at the stage of history taking is especially important for making a correct final diagnosis among students. Research has revealed that students who make the correct diagnosis at the end of history taking are more likely to reach a correct final diagnosis than those who fail to do so. To improve diagnostic reasoning skills among medical students, they should be trained in the ability to infer the correct diagnosis from the case history.[6]
This also calls for training in communication skills as an essential component of medical education and as a matter of fact, training in communication skills has become an essential component of medical education worldwide.[8]
Today’s patient is an informed consumer who has open access to information which was previously restricted to doctors. The patient – doctor clinical encounter is a co-operative interaction which culminates in an agreement about what ails the patient and what the doctor can do in response. The sociology of diagnosis plays an important role in understanding the illness and identifying the priorities and goals of intervention.[9] Clinical decision making for a beneficial outcome is best based on a timely and accurate diagnosis and this in turn is dependent on a comprehensive study of a patient’s health issues.[4]
The Committee on Diagnostic Error in Health Care identified four types of information-gathering activities in the diagnostic process: taking a clinical history and interview; performing a physical exam; obtaining diagnostic testing; and sending a patient for referrals or consultations.[10] In the process of information collection and collation, there is a need for health care professionals to communicate effectively with the patient and his / her family, keeping in view the patients’ culture, values and choices.[10] A common adage in medicine ascribed to William Osler is: “Just listen to your patient, he is telling you the diagnosis”.[11]
The need to train the medico in communication skills during the MBBS curriculum is explicitly commended by the “Vision 2015” document of the Medical Council of India. It is also a challenge to ensure that students not only imbibe the nuances of communication and interpersonal skills, but adhere to them throughout their careers.[12]
Difficulties in gathering the patient’s relevant and comprehensive history may be due to the patient being unable to communicate (older adults, children etc.), lack of sufficient time for the medical interview etc. In many situations, inclusion of the family members or caregivers in the history-taking process becomes necessary. Ensuring a safe milieu for patients and a sensitive approach to encourage them to divulge delicate and personal information about their health condition is a responsibility of the health professional. An incomplete picture of a patient's relevant history and current signs and symptoms may lead to diagnostic errors and subsequent poor treatment outcomes.[10]
In recent years due to the explosion of laboratory testing and imaging, what was once the primary means of diagnosis i.e., the history and physical examination are being bypassed by physicians and the same is being communicated indirectly to the student. Thus, there is a risk of missing the diagnosis of simple diseases and even worse hampering the physician–patient relationship.[13]
“Overuse” is a term in medical practice which refers to the delivery of tests and procedures that provide little or no clinical benefits. While clinicians are responsible for this overuse, their practice patterns may be influenced by hospital policies and culture.[14] Diagnostic cascade is a phenomenon that points to unnecessary testing which may lead to false positive results, thereby leading to more tests. [15]
Belittling the importance of the history and examination is evident by the act of handing patients their medical records (especially their OP record) when they leave the clinic / hospital. Medical records have to be kept carefully in the hospital for a specified period of time for not only the continuity of care but also evaluation and review of patient management issues, analyzing treatment results, to plan treatment protocols and as documentary evidence in issues of alleged medical negligence.[16] This study is set to look at the perceptions and skills of medical students concerning history taking, physical examination and communication as the first line of patient diagnosis.
Objectives
To identify the importance given to history taking in disease diagnosis among medicos.
To compare attitudes towards history taking, physical examination and communication with patients.
Materials and Methods
This descriptive study was done over a period of 2 months involving 164 medicos (110 final years and 54 interns) in NRI Medical College. After informed consent, a predetermined questionnaire on history taking and other modes of diagnosis was administered. The collected data was entered and analyzed in Microsoft Excel. Important findings were subjected to tests of significance like Chi square at 5% Level of significance.
|
S. No |
Observations |
Total (n = 164) No. (%) |
Final year (n = 110) No. (%) |
Intern (n = 54) No. (%) |
Chi Sq |
p value |
|
1 |
Diagnosis is the most important function of an MBBS doctor |
72 (43.9) |
49 (44.5) |
23 (42.6) |
0.06 |
0.81 |
|
2 |
One can make a good diagnosis by history alone |
22 (13.4) |
14 (12.7) |
8 (14.8) |
0.14 |
0.71 |
|
3 |
History and examination together can give 90% accurate diagnosis |
75 (45.7) |
50 (45.5) |
25 (46.3) |
0.01 |
0.92 |
|
4 |
Investigations are mainly for documentation & prognosis |
48 (29.3) |
35 (31.8) |
13 (24.1) |
1.05 |
0.31 |
|
5 |
At least 20 minutes is needed for patient interview during first visit |
44 (26.8) |
30 (27.3) |
14 (25.9) |
0.03 |
0.85 |
|
6 |
History includes patient personal, social & financial aspects |
66 (40.2) |
46 (41.8) |
20 (37.0) |
0.34 |
0.56 |
|
7 |
Relevant questions in history will give the complete picture |
70 (42.7) |
43 (39.1) |
27 (50.0) |
1.76 |
0.18 |
|
8 |
It is necessary to give relevant health information to the patient |
66 (40.2) |
42 (38.2) |
24 (44.4) |
0.59 |
0.44 |
|
9 |
Too much time on history and examination is a time waste |
10 (6.1) |
6 (5.5) |
4 (7.4) |
0.24 |
0.62 |
|
S. No. |
Observations |
Total (n = 164) No. (%) |
Final year (n = 110) No. (%) |
Intern (n = 54) No. (%) |
Chi Sq |
p |
|
1 |
MBBS is the best time to learn history taking skills |
77 (47.0) |
48 (43.0) |
29 (53.7) |
1.47 |
0.22 |
|
2 |
Communication is an important skill to learn during MBBS |
37 (22.6) |
26 (23.) |
11 (20.4) |
0.22 |
0.64 |
|
3 |
Role plays on history taking will help in learning the skill |
40 (24.4) |
18 (16.4) |
22 (40.7) |
11.70 |
0.0006 |
|
4 |
Workshops on history taking skills needed in MBBS curriculum |
55 (33.5) |
35 (31.8) |
20 (37.0) |
0.44 |
0.51 |
|
5 |
Feedback about doctor-patient communication is necessary |
43 (26.2) |
28 (25.4) |
15 (27.8) |
0.10 |
0.75 |
|
6 |
Doctors must deal with patient's emotions during interview |
75 (45.7) |
55 (50.0) |
20 (37.0) |
2.45 |
0.12 |
|
7 |
Confident in taking a good history from the patient |
12 (7.3) |
9 (8.2) |
3 (5.6) |
0.37 |
0.54 |
|
8 |
Have taken and presented sufficient cases |
8 (4.9) |
5 (4.5) |
3 (5.6) |
0.08 |
0.78 |
|
S.No |
Questions |
Total (n = 164) No. (%) |
Males (n = 60) No. (%) |
Females (n = 104) No. (%) |
Chi Sq |
p |
|
1 |
Diagnosis is the most important function of an MBBS doctor |
72 (43.9) |
38 (63.3) |
34 (32.7) |
14.50 |
0.0001 |
|
2 |
One can make a good diagnosis by history alone |
22 (13.4) |
11 (18.3) |
11 (10.6) |
1.97 |
0.16 |
|
3 |
History and examination together can give 90% accurate diagnosis |
75 (45.7) |
31 (51.7) |
44 (42.3) |
1.34 |
0.25 |
|
4 |
Investigations are mainly for documentation & prognosis |
48 (29.3) |
22 (36.7) |
26 (25.0) |
2.50 |
0.11 |
|
5 |
At least 20 minutes needed for 1st visit patient interview |
44 (26.8) |
19 (31.7) |
25 (24.0) |
1.13 |
0.29 |
|
6 |
History includes patient personal, social & financial aspects |
66 (40.2) |
29 (48.3) |
37 (35.6) |
2.57 |
0.11 |
|
7 |
Relevant questions in history will give the complete picture |
70 (42.7) |
32 (53.3) |
38 (36.5) |
4.39 |
0.04 |
|
8 |
It is necessary to give patient relevant health information |
66 (40.2) |
30 (50.0) |
36 (34.0) |
3.74 |
0.05 |
|
9 |
Too much time on history and examination is a waste |
10 (6.1) |
6 (10.0) |
4 (3.8) |
2.52 |
0.11 |
|
S. No |
Questions |
Total (n = 164) No. (%) |
Males (n = 60) No. (%) |
Females (n = 104) No. (%) |
Chi Sq |
p |
|
1 |
MBBS is the best time to learn history taking skills |
77 (47.0) |
34 (56.7) |
43 (41.3) |
3.59 |
0.05 |
|
2 |
Communication is an important skill to learn during MBBS |
37 (22.6) |
10 (16.7) |
27 (26.0) |
1.88 |
0.17 |
|
3 |
Role plays on history taking will help in learning the skill |
40 (24.4) |
20 (33.3) |
20 (19.2) |
4.10 |
0.04 |
|
4 |
Workshops on history taking skills needed in MBBS curriculum |
55 (33.5) |
22 (36.7) |
33 (31.7) |
0.42 |
0.52 |
|
5 |
Feedback about doctor-patient communication is necessary |
43 (26.2) |
18 (30.0) |
25 (24.0) |
0.70 |
0.40 |
|
6 |
Doctors must deal with patient's emotions during interview |
75 (45.7) |
35 (58.3) |
40 (38.5) |
6.05 |
0.01 |
|
7 |
Confident in taking a good history from the patient |
12 (7.3) |
6 (10.0) |
6 (5.8) |
1.00 |
0.32 |
|
8 |
Have taken and presented sufficient cases |
8 (4.9) |
4 (6.7) |
4 (3.8) |
0.65 |
0.42 |
Results
63.3% men and 32.7% women (total 43.9%) strongly agreed that diagnosis is one of the most important functions of doctor ([Table 3]). Only 18.3 % of the men and 10.6 % of the women were convinced that a good diagnosis was possible with case taking alone. Only 14.8% of the Interns and 12.7% of the students strongly felt that case history alone could give a good diagnosis. ([Table 1]). However, only 4.9% medicos (6.7% males and 3.8% females) said that they presented sufficient number of case histories during their undergraduate medical course ([Table 3]). 10.0 % males and 3.8% females felt that time spent on history taking was not a waste (Chi square 10.95, p value <0.001). Only 22.6 % of the medicos thought that communication was an important skill in patient care ([Table 4]). Overall, 7.3 % of the medicos felt confident in taking a good history. 61% of the medicos agreed that the OP record with history, examination findings and investigation results can be handed over to the patient to take home while another 45 (27.4%) were not sure.
Discussion
Making a diagnosis is a key skill to be learned by all medicos during their undergraduate medical course. To make a diagnosis, the medical student is taught to take a very detailed history followed by a physical examination. With these two tools, the student is encouraged to make a positive diagnosis (with a few differential diagnoses) all through the clinical years of teaching. It is only in the internship that a medical student grapples with the collection of specimens for investigations and collecting the results so that the physicians in the unit can decide how to treat the patient. Unfortunately, in today’s medical world, the undergraduate student hardly has time to rationally think and apply his knowledge to a particular problem. There is a lot to learn and a multitude of internal assessments and examinations. The pursuit of increasing book-based knowledge takes precedence over picking up practical skills and attitudes.
A medical student must not only learn what is written in the textbooks, but also spend much time in observing and practicing skills like case taking and physical examination in order to gain confidence in patient care.[17] In this study it is seen that most medicos did not present sufficient cases during their course and most of them were not confident about their history taking skills. In today’s commercial medical world, employing a technician to undertake a battery of investigations seems more cost-effective compared to using expensive clinician time listening to patients.[18] However, it would be judicious to design the MBBS curriculum with an appropriate balance between history taking and other diagnostic modalities.
Hampton JR et al. in their study found that history alone helped in making a good diagnosis in 82.5% of new patients. They found that just a small number of patients needed further laboratory investigations for diagnosis.[18] With a robust medical history, in many instances, it becomes clear that investigations are superfluous.[19]
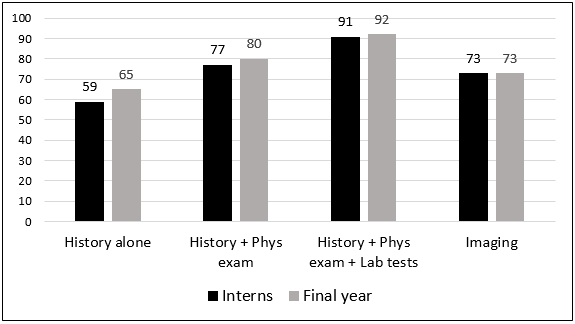
Peterson MC et al. suggest from their study that most diagnoses are made from the medical history. In their study, they found that 76% of the patients could be diagnosed accurately by history alone, 12% by the physical examination and 11% needed laboratory investigations. The physician’s confidence in the correct diagnosis increased from 7.1 on a scale of 1 to 10 after the history to 8.2 after the physical examination and 9.3 after the laboratory investigation.[20] In the current study too, medicos have shown their perceptions regarding diagnostic accuracy using the above tools ([Figure 1]). We suggest the appropriate use of diagnostic tools in the manner given in [Figure 2].
The current study indicates the effect of needing investigations to make a diagnosis among medicos is gradually eroding the importance of history taking and physical examination. This is seen by the fact that very few medicos are presenting cases in the clinics. Communication with the patient is also seen as not necessary.
Bakarman MA et al. in their study found that the utilization of laboratory tests was inappropriate in 51% of the cases of which 13.2% were subject to over utilization of lab testing.[21] Investigation centered diagnosis is associated not only with increased costs but also with direct physical risks due to some of the more invasive investigations.[19]
Coming to medical records, the Out Patient (OP) record is not only the point of first contact of a patient but is also a continuing record of all the patient’s visits. It has legal value and also provides continuity of care. Just as the inpatient record, the OP record also cannot be given to the patient to take home.[16]
Seitz T et al. found in their study involving physicians in charge of training medicos that the medical students lacked the expertise and ability to take a structured and complete medical history. They suggest that there is a need for a refinement of the training of communicative skills and practical training for them.[22] The traditional approach to teaching history taking in medical colleges is to use focused scripts with emphasis on content and completeness. A review of a video of a student-patient case taking interview can help in identifying subtle communication issues. Online video demonstrations, text modules on communication, learning by doing approach-based workshops are very effective methods. Small group sessions involving simulated or real patients with role-plays and feedback are other methods. Assessment of history taking skills can be done with students’ self-evaluation questionnaires, written reflections, real time or videotaped observation by trained observers, use of checklists or Objective Structured Clinical Examination (OSCE) stations.[3]
Often, in the quest for a diagnosis, we find that more information can be gained during the clinical history and physical examination than a battery of investigations. Efforts must be made to refine the art of history taking, as it narrows the focus of the physical examination thereby leading to an accurate diagnosis.[23]
Conclusion
A good clinical history provides adequate and appropriate information and is therefore the first important step in making a diagnosis in clinical practice.[24] The history not only helps the physician to understand why the patient came to the hospital, as well as the biological, psychological and social context that led to the presenting issue. Undergraduate medical education must ensure training in good communication with patients and reliance on history taking and examination skills for diagnosis. Small-group skills workshops using role-plays with simulated or real patients followed by effective feedback are definite ways to certifiable training in medical colleges.
Source of Funding
None.
Conflict of Interest
None.
References
- WL Morgan, GL Engel, MN Luria. The general clerkship: a course designed to teach the clinical approach to the patient. J Med Educ 1972. [Google Scholar]
- JR Nichol, JH Sundjaja, G Nelson. Medical History. Stat Pearls 2021. [Google Scholar]
- KE Keifenheim, M Teufel, J Ip, N Speiser, EJ Leehr, S Zipfel. Teaching history taking to medical students: a systematic review. BMC Med Educ 2015. [Google Scholar]
- ES Holmboe, SJ Durning. Assessing clinical reasoning: moving from in vitro to in vivo. Diagnosis 2014. [Google Scholar]
- JH Lai, KH Cheng, YJ Wu. Assessing clinical reasoning ability in fourth-year medical students via an integrative group history-taking with an individual reasoning activity. BMC Med Educ 2022. [Google Scholar]
- T Tsukamoto, Y Ohari, K Noda, T Takada, M Ikusaka. The contribution of the medical history for the diagnosis of simulated cases by medical students. Int J Med Educ 2012. [Google Scholar]
- LD Gruppen, NS Palchik, FM Wolf, TJ Laing, M S Oh, WK Davis. Medical student use of history and physical information in diagnostic reasoning. Arthritis Care Res 1993. [Google Scholar]
- S Kurtz, J Silverman, J Benson, J Draper. Marrying content and process in clinical method teaching: enhancing the Calgary- Cambridge guides. Acad Med 2003. [Google Scholar]
- A Jutel. Sociology of diagnosis: a preliminary review. Sociol Health Illness 2009. [Google Scholar]
- Engineering, EP Balogh, BT Miller, JR Ball. Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences. The Diagnostic Process 2015. [Google Scholar]
- JS Gandhi, W Osler. A Life in Medicine. BMJ 2000. [Google Scholar]
- JN Modi, AJ Chhatwal, P Gupta, T Singh. Teaching and Assessing Communication Skills in Medical Undergraduate Training. Indian Pediatrics 2016. [Google Scholar]
- A Verghese, E Brady, CC Kapur, RI Horwitz. The Bedside Evaluation: Ritual and Reason. Ann Int Med 2011. [Google Scholar]
- K Chalmers, P Smith, J Garber. Assessment of Overuse of Medical Tests and Treatments at US Hospitals Using Medicare Claims. JAMA Netw Open 2021. [Google Scholar]
- C Koch, K Roberts, C Petruccelli, DJ Morgan. The Frequency of Unnecessary Testing in Hospitalized Patients. Am J Med 2018. [Google Scholar]
- J Thomas. Medical records and issues in negligence. Indian J Urol 2009. [Google Scholar]
- M Guragai, D Mandal. Five Skills Medical Students Should Have. J Nepal Med Assoc 2020. [Google Scholar]
- JR Hampton, MJ Harrison, JR Mitchell, JS Prichard, C Seymour. Relative contributions of history-taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients. Br Med J 1975. [Google Scholar]
- N Summerton. The medical history as a diagnostic technology. Br J Gen Pract 2008. [Google Scholar]
- MC Peterson, JH Holbrook, V Hales, D Smith, NL Staker. Contributions of the history, physical examination, and laboratory investigation in making medical diagnoses. West J Med 1992. [Google Scholar]
- MA Bakarman, NY Kurashi, M Hanif. Utilization of laboratory investigations in primary health care centers in Al-khobar, Saudi Arabia. J Family Commun Med 1997. [Google Scholar]
- T Seitz, B Raschauer, AS Längle. Löffler-Stastka H, Competency in medical history taking-the training physicians' view. Wien Klin Wochenschr 2019. [Google Scholar]
- JC Muhrer. The importance of the history and physical in diagnosis. . Nurse Pract 2014. [Google Scholar]
- B Lown. . The lost art of healing: practicing compassion in medicine 1999. [Google Scholar]
How to Cite This Article
Vancouver
Indu K, Rao NSS. Importance of case history in disease diagnosis as perceived by medicos [Internet]. South Asian J Health Prof. 2025 [cited 2025 Sep 06];7(2):37-42. Available from: https://doi.org/10.18231/j.sajhp.2024.009
APA
Indu, K., Rao, N. S. S. (2025). Importance of case history in disease diagnosis as perceived by medicos. South Asian J Health Prof, 7(2), 37-42. https://doi.org/10.18231/j.sajhp.2024.009
MLA
Indu, K., Rao, N. S. Sanjeeva. "Importance of case history in disease diagnosis as perceived by medicos." South Asian J Health Prof, vol. 7, no. 2, 2025, pp. 37-42. https://doi.org/10.18231/j.sajhp.2024.009
Chicago
Indu, K., Rao, N. S. S.. "Importance of case history in disease diagnosis as perceived by medicos." South Asian J Health Prof 7, no. 2 (2025): 37-42. https://doi.org/10.18231/j.sajhp.2024.009
