Introduction
Hodgkin’s lymphoma (HL) is a common, malignant hematological tumor of the lymph nodes (LN) and lymphatic system, accounting for approximately 10% of all lymphomas. HL comprises 2 main subtypes: (1) classical HL (cHL) and (2) nodular lymphocyte predominant HL.
There are no clearly defined risk factors for the development of this disease and the cause of HL remains unknown. Factors shown to be associated with HL include familial factors, viral exposures, and immune suppression.
Epstein-Barr virus is a risk factor for the development HL, upto 40 % cases are associated with infection. Epidemiologic and serologic studies have implicated Epstein–Barr virus (EBV) in the etiology of HL and the EBV genome was been detected in tumor specimens from patients with HL. There is also an association with human immunodeficiency (HIV) infection, in that HIV-infected patients have a significantly increased risk of HL when compared to the general population.
The JAK/STAT signaling pathway is also critically involved in Typical HL pathogenesis. Epstein-Barr virus nuclear antigen-1 (EBNA1) is also positive in affected cells.1, 2
Table 1
Difference between NHL & HL: Classical Hodgkins disease (cHD) makes 95% cases.3
Table 2
Symptoms of hodgkins lymphoma4
Patients with Hodgkin lymphoma have been shown to have high levels of antibodies against Epstein-Barr virus. HIV-1 is a human carcinogen that causes Hodgkin lymphoma via immunosuppression (indirect action). Association with tobacco smoking is controversial.5
Table 3
Classification of hodgkins lymphoma6
Table 4
Poor prognosis in hodgkins lymphoma6
Table 5
Diagnostic workup on hodgkins lymphoma 7
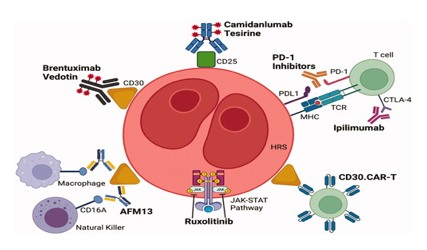
Timeline history of FDA Approvals in Hodgkin lymphoma
(Adapted Fig from : Hazane Leroyer, E.; Ziegler, C.; Moulin, C.; Campidelli, A.; Jacquet, C.; Rubio, M.T.; Feugier, P.; Pagliuca, S. Filling the Gap: The Immune Therapeutic Armamentarium for Relapsed/Refractory Hodgkin Lymphoma. J. Clin. Med. 2022, 11, 6574. https://doi.org/10.3390/ jcm11216574)
Chemotherapy of Hodgkins Lymphoma
First Line Chemotherapy for Classical HD
ABVD: Doxorubicin, bleomycin , vinblastine and dacarbazine. ABVD chemotherapy is usually given every 2 weeks for 2 to 8 months.
AAVD: This regimen is similar to ABVD, but brentuximab vedotin replaces bleomycin. AAVD is given every 2 weeks for 6 months.
BEACOPP: Bleomycin, etoposide, doxorubicin, cyclophosphamide vincristine procarbazine and prednisone. There are several different treatment schedules, but different drugs are usually given every 2 to 3 weeks.
Second Line Chemotherapy or reserve regimens
ICE: Ifosfamide , carboplatin, and etoposide. ICE is usually given every 2 or 3 weeks for 2 to 3 cycles.
Brentuximab vedotin It is usually given every 3 weeks for up to 16 cycles
GVD: GVD is gemcitabine, vinorelbine (Navelbine, and doxorubicin.
ESHAP is etoposide, methylprednisolone, high-dose cytarabine, and cisplatin.
DHAP is dexamethasone, high-dose cytarabine, and cisplatin.
Other Therapies: Immunotherapy: Nivolumab and pembrolizumab, Radiation therapy - gold standard for external beam RT is 3D-CRT that use a linear accelerator (LINAC). Involved-site radiation therapy (ISRT) is sometimes preferred treat HL. It selectively treats the lymph nodes where the cancer started. External beam radiation therapy is provided 15 to 20 minutes and is typically administered five days a week for several weeks. Autologous transplantation of stem-cells is a therapeutic option for Hodgkin's lymphoma patients after the first relapse. Promising results were observed in patients with a low tumor burden at transplant.8, 9
Table 6
Traditional drug monotherapy for hodgkins lymphoma 10
Biologicals for Hodgkins Disease
Brentuximab vedotin is composed of 3 parts: a chimeric human-murine IgG1 that selectively targets CD30, monomethyl auristatin E (MMAE), which is a microtubule-disrupting agent, and a protease-susceptible linker that links the antibody and MMAE. Brentuximab vedotin causes apoptosis of tumor cells by preventing cell cycle progression of the G2 to M phase.
Brentuximab vedotin having half life between 4- 6 days, is indicated in adult patients for the treatment of previously untreated stage III or IV classical Hodgkin's lymphoma (cHL) in combination with doxorubicin, vinblastine, and dacarbazine. Frontline treatment with the combination of brentuximab vedotin, nivolumab, doxorubicin, and dacarbazine led to an overall response rate ORR of 98%. The most severe toxic reaction observed is progressive multifocal leukoencephalopathy.11
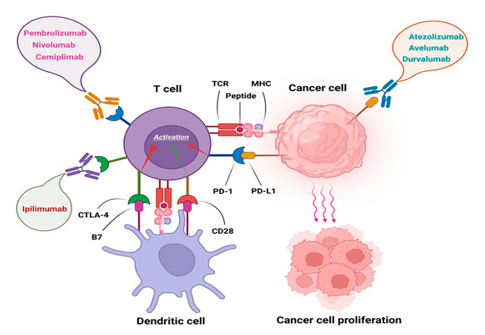
Nivolumab The ligands PD-L1 and PD-L2 bind to the PD-1 receptor on T-cells, inhibiting the action of these cells. Tumor cells express PD-L1 and PD-L2. Nivolumab, Pembrolizumab binds to PD-1, preventing PD-L1 and PD-L2 from inhibiting the action of T-cells, restoring a patient's tumor-specific T-cell response.
Nivolumab, an anti-PD-1 monoclonal antibody, demonstrated durable responses and manageable toxicity in a significant population of HL patients who fail both ASCT and brentuximab vedotin.
Brentuximab vedotin plus nivolumab was highly active post-autologous HSCT consolidation for patients with high-risk relapsed or refractory classic Hodgkin lymphoma, most of whom had previous exposure to either brentuximab vedotin or PD-1 blockade.12
Pembrolizumab combination with Brentuximab is a highly effective and safe bridge treatment to ASCT for high-risk, heavily pretreated R/R HL patients. 13
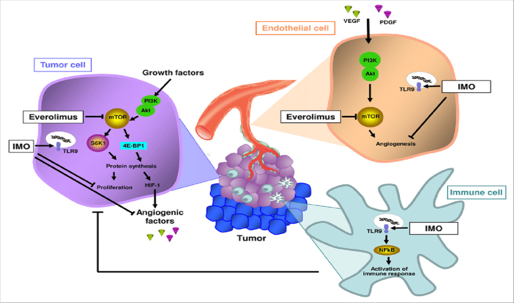
Everolimus is a mTOR inhibitor that binds with high affinity to the FK506 binding protein-12 (FKBP-12), thereby forming a drug complex that inhibits the activation of mTOR. This inhibition reduces the activity of effectors downstream, which leads to a blockage in the progression of cells from G1 into S phase, and subsequently inducing cell growth arrest.
Everolimus was found to provide a response in a group of patients with refractory or relapsed Hodgkin's lymphoma who had adequate tolerability to the drug.14
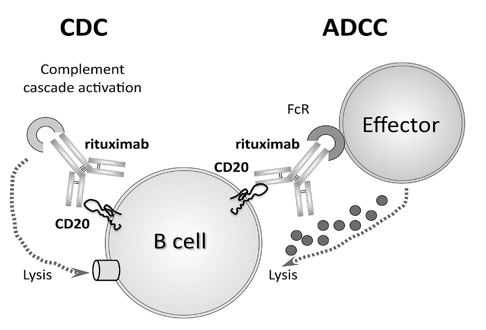
Rituximab: binds specifically to the CD20 antigen located on pre-B and mature B lymphocytes1 Because they lack CD20, stem cells and plasma cells are not selectively targeted by Rituximab. rituximab is often used to treat variant of Hodgkin lymphoma called 'nodular lymphocyte-predominant Hodgkin lymphoma' (NLPHL).15
Bortezomib (inhibits nuclear factor kappa B (NF-κB) with ifosfamide and vinorelbine are evaluated in childhood Hodgkins disease.
Panobinostat, Mocetinostat , Entinostat are oral nonhydroxamate HDAC inhibitors that selectively inhibits Histone deacetylases 1, 2, 3 used in refractory HL. In some cases.
Panobinostat as a single agent produced an overall response rate of 27% in patients with relapsed or recurrent Hodgkin lymphoma after stem cell transplantation.16, 17, 18
Lucatumumab, a human anti-CD40 mAb, was shown to cause more B-cell lysis than rituximab, by targeting CD4O. Galiximab, a primatized immunoglobulin G 1 monoclonal antibody against CD80, has high affinity binding for CD80 and induces antibody-dependent cytotoxicity (ADCC}. Mogamulizumab selectively binds to and inhibits the activity of CCR4, which may block CCR4-mediated signal transduction pathways, is being evaluated for refractory HL.
Conclusion
The major cause of HL is change in make up of DNA of white blood cells. called B lymphocytes. There is B Cell downregulation. 80%–90% of HL patients achieve permanent remission and can be considered cured. Hodgkin lymphoma has high cure either by chemotherapy or chemoradiation. Addition of immunotherapies to established chemotherapy results in improved outcomes in terms of toxicity. Chimeric antigen receptor (CAR) T-cell therapy has provided a curative option for patients with relapsed or refractory lymphoma. CD30 is an appropriate target for CAR-T-cell therapy of patients with HL. CD19 and CD123 CAR T cells that target the immunosuppressive tumor microenvironment in HL have also been investigated. Secondary malignancies such as solid tumors (lung, breast), cardiovascular disease, hypothyroidism, and fertility issues are late effects in long-term complications of HL. Vinorelbine, Idarubicin, Gemcitabine and Immunotherapy have been evaluated in resistant cases. The disease is aggressive in older patients with poor response rate. The 5 year relative survival rate is 89 %., compared to 74% of Non Hodgkins lymphoma. High-dose chemotherapy and autologous stem-cell transplant (HDC/ASCT) is standard treatment for chemo sensitive relapsed classical Hodgkin lymphoma. The current standard of care for early stage HL is two cycles of ABVD and 20 Gy radiotherapy for favourable prognosis, and four cycles of ABVD and 30 Gy for unfavourable prognosis. The standard of care for advanced HL in patients aged 16 to 60 is either 6-8 cycles of ABVD or six cycles of eBEACOPP.