- Visibility 123 Views
- Downloads 19 Downloads
- DOI 10.18231/j.sajhp.2023.005
-
CrossMark
- Citation
Surgical management of oral squamous cell carcinoma of the lower gingivobuccal complex: A case report
Introduction
Oral cancers account for about 10.3% of cancers according to Globocan 2020.[1] The incidence of oral cancer is higher in India than in western countries due to the high prevalence of tobacco use. 90% of these comprise oral squamous cell carcinoma (OSCC). Given the fact that a major portion of tobacco users place the tobacco quid in the vestibular region, the gingivobuccal complex is the most common site for the development of oral cancers.[2]
Anatomically, the close positioning of cancers developing in these sites with the mandibular jawbone predisposes them toward tumour invasion and metastasis. Therefore, a multidetector CT (MDCT) scan is fairly reliable in the preoperative assessment of mandibular invasion and estimation of the level of involvement.[3]
Managing such tumours necessitates not only astute clinical judgement but also precise imaging and a full understanding of the biology of tumour dissemination paths. Despite the fact that radical excision with adjuvant radiotherapy is the conventional treatment, advanced gingivobuccal tumours have extremely high locoregional failure rates.[4] The current case report describes the presentation and management of OSCC of the lower gingivobuccal complex.
Case Report
A 65-year-old male complained of pain in the lower left posterior teeth region of the oral cavity for the past three months. The pain was intermittent and dull, aggravated while brushing teeth and bleeding from the gingiva of the involved area. He also experienced a burning sensation in the oral cavity on consuming hot or spicy foods. The patient’s medical history was unremarkable while a habit history of bidi smoking for the past 20 years and alcohol intake for 25 years was elicited.
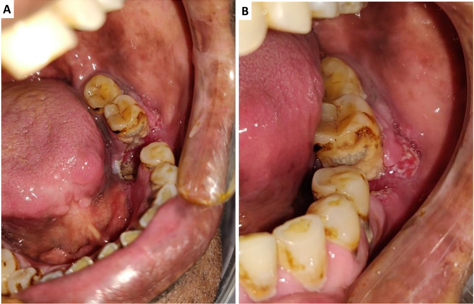
Extraoral examination revealed multiple painful sub mandibular and upper cervical groups of lymph nodes which were approximately 3 cm in diameter. Intraorally, an ulcer proliferative lesion was present involving the gingivobuccal area. In the mandibular left premolar-molar region. The lesion was found to be associated with tenderness and mild induration on palpation. ([Figure 1]). The involved teeth also exhibited Grade III mobility and profuse bleeding was noted on gingival probing of the same. The oral hygiene status was poor as evidenced by generalized heavy stains and subgingival calculus deposits.
An MDCT scan of the head and neck showed the existence of a focused area of bony destruction involving the left mandibular bony alveolus at the left molar region with a missing molar. The defect was roughly 23x22 mms in size. It also involved the left floor of the mouth close to the left lower alveolar mucosa. Two enlarged left bottom 1b nodes measuring 22x14 and 21x14.6 mms were detected. Parotid and submandibular salivary glands were typical in size, with no aberrant attenuation. The nasopharynx, oropharynx, and hypopharynx were all normal, with very minor signs of cervical spondylosis.
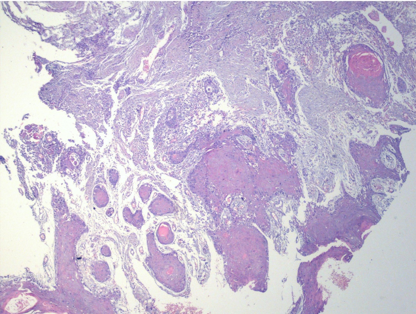
An incisional biopsy was obtained and on microscopic examination, neoplastic epithelial cells infiltrating the underlying connective tissue in the form of numerous islands and sheets were noted ([Figure 2]). The cells exhibited moderate nuclear pleomorphism and about 1-2 mitotic figures per high power field. Abundant keratin pearls were present within the connective tissue stroma. Based on clinical, radiological, and histological features, the final diagnosis was confirmed as squamous cell carcinoma of the gingivobuccal complex. The clinical staging of the present case was discerned as T4aN1M0 while the pathological stage was stage IV A-PT4a, PN1 according to the AJCC system of staging tumours because of the involvement of jaw bone and palpable lymph nodes of size more than 2 cm.
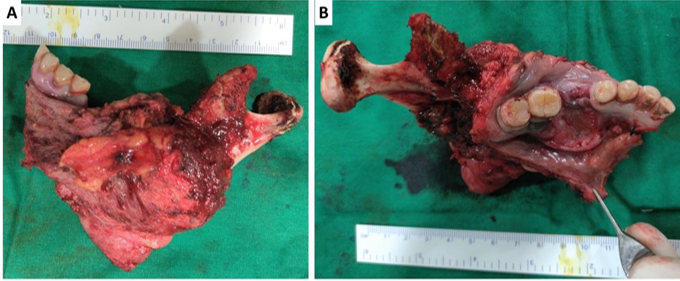
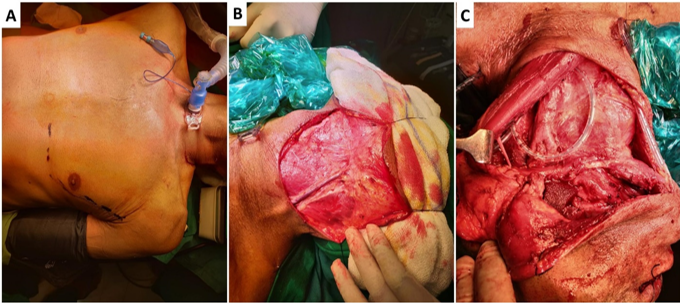
The patient was draped under strict aseptic conditions and precautions and a tracheostomy was performed followed by endotracheal intubation. Neck dissection was accomplished using a single apron incision. By opening the neck and ligating the facial artery, a clear surgical field was obtained. Neck dissection (Level I-V) was performed unilaterally. To maintain adequate mouth opening, a cheek retractor and biting block were put between the opposing molars. A border of 1.5 cm was marked around the lesion prior to its resection. Resection was completed with the 3-dimensional extent of the lesion in mind. The lesion and involved floor of mouth were excised orally together with hemimandibulectomy, and the specimen was delivered through neck dissection. ([Figure 3]). The resected specimen was evaluated to ensure that the surgical resection margins were appropriate and to determine the need for additional resection. The defect was then reconstructed with Pectoralis major myocutaneous flap ([Figure 4]). Adjuvant radiation therapy was recommended for the patient.
Discussion
OSCC is the most frequent type of oral malignant neoplasm, accounting for 96% of all malignant tumours in this area.[5] This is associated with the chewing of dried and cured tobacco leaves, betel nut, and slaked lime. This mixture is extremely irritating to the oral mucosa and causes a wide range of diseases, from premalignant lesions to full-blown cancers.[6]
OSCCs of the gingivobuccal complex cancers are a homogeneous group of tumours in terms of mandibular invasion, with tumour entrance preferentially through the occlusal surface. An MDCT scan is fairly reliable in the preoperative assessment of mandibular invasion and estimation of the level of involvement of other tissues including the lymph nodes. Large tumours with para-mandibular involvement are likely to have many entry points, which contradicts mandibular conservation.[7]
The goal of surgical resection is to remove the entire primary cancer with clean tumour-free margins in three dimensions. Hemimandibulectomy is advised only when there is severe involvement of the mandible by cancer, perineural invasion by the tumour, and the presence of massive dissemination of the tumour in the para mandibular area.[8] In the absence of clinically positive neck, supra omohyoid neck dissection eliminating I, II, and III lymph node levels are sufficient and alleviates morbidity. However, a thorough neck dissection from Level I to Level V is required for a clinically positive neck.
Depending on the extent of resection, the patient's health, willingness, past treatment, socioeconomic factors, and competence available, reconstructive choices range from leaving a raw post-CO2 laser excision area to elaborate microvascular reconstructions.[9]
Conclusion
Management of OSCC requires generous clinicoradiological and histopathological investigations, followed by prompt treatment so as to reduce morbidity, avoid spread and subsequent complications. A thorough resection would ensure reduced chances of recurrence. The present case report would serve to guide clinicians in the decision-making aspect during the management of extensive gingivobuccal OSCC.
Source of Funding
None.
Conflict of Interest
None.
References
- H Sung, J Ferlay, RL Siegel, M Laversanne, I Soerjomataram, A Jemal. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021. [Google Scholar]
- JO Christopher, TJ Brien. Epidemiology in head and neck cancer. Curr Opin Oncol 2009. [Google Scholar]
- RR Walvekar, DA Chaukar, MS Deshpande, PS Pai, P Chaturvedi, A Kakade. Squamous cell carcinoma of the gingivobuccal complex: Predictors of locoregional failure in stage III-IV cancers. Oral Oncol 2009. [Google Scholar]
- KA Pathak, S Gupta, S Talole, V Khanna, P Chaturvedi, MS Deshpande. Advanced squamous cell carcinoma of lower gingivobuccal complex: patterns of spread and failure. Head Neck 2005. [Google Scholar]
- LA Cabral, LF De Carvalho, JA Salgado, AA Brandão, JD Almeida. Gingival squamous cell carcinoma: a case report. J Oral Maxillofac Res 2010. [Google Scholar] [Crossref]
- SA Pradhan. Surgery for cancer of the buccal mucosa. Semin Surg Oncol 1989. [Google Scholar]
- D A Chaukar, M Dandekar, S Kane, S Arya, N Purandare, V Rangarajan, D' Cruz, A K. Invasion of the mandible in gingivobuccal complex cancers: Histopathological analysis of routes of tumour entry and correlation with preoperative assessment. Oral Oncology 2018. [Google Scholar]
- D S Mandlik, S S Nair, K D Patel, K Gupta, P Patel, P Patel, N Sharma, A Joshipura, M Patel. Squamous cell carcinoma of gingivobuccal complex: Literature, evidences and practice. Journal of Head & Neck Physicians And Surgeons 2018. [Google Scholar]
- H Chim, C J Salgado, R Seselgyte, F C Wei, S Mardini. Principles of head and neck reconstruction: An algorithm to guide flap selection. Semin Plast Surg 2010. [Google Scholar]
How to Cite This Article
Vancouver
Wadewale M, Chhapane A, Sachdev SS, Latke S, Kalamkar J. Surgical management of oral squamous cell carcinoma of the lower gingivobuccal complex: A case report [Internet]. South Asian J Health Prof. 2025 [cited 2025 Sep 04];6(1):22-24. Available from: https://doi.org/10.18231/j.sajhp.2023.005
APA
Wadewale, M., Chhapane, A., Sachdev, S. S., Latke, S., Kalamkar, J. (2025). Surgical management of oral squamous cell carcinoma of the lower gingivobuccal complex: A case report. South Asian J Health Prof, 6(1), 22-24. https://doi.org/10.18231/j.sajhp.2023.005
MLA
Wadewale, Maroti, Chhapane, Ashwini, Sachdev, Sanpreet Singh, Latke, Siddhesh, Kalamkar, Jayashree. "Surgical management of oral squamous cell carcinoma of the lower gingivobuccal complex: A case report." South Asian J Health Prof, vol. 6, no. 1, 2025, pp. 22-24. https://doi.org/10.18231/j.sajhp.2023.005
Chicago
Wadewale, M., Chhapane, A., Sachdev, S. S., Latke, S., Kalamkar, J.. "Surgical management of oral squamous cell carcinoma of the lower gingivobuccal complex: A case report." South Asian J Health Prof 6, no. 1 (2025): 22-24. https://doi.org/10.18231/j.sajhp.2023.005
