Introduction
A woman presenting with vulvo vaginal lesions is to be examined and evaluated further before giving her the definitive diagnosis and proposing treatment. As the differential diagnosis may vary from benign lesions like lichen sclerosus, vulval intraepithelial neoplasia or malignant lesions like squamous cell carcinoma. We are presenting a case report wherein 70 year woman presented with features similar to squamous cell carcinoma but was diagnosed as pseudoepitheliomatous hyperplasia of vulva which is a benign lesion.
Pseudoepitheliomatous hyperplasia (PEH) is a benign condition, characterized by hyperplasia of the epidermis and adnexal epithelium, closely simulating squamous cell carcinoma.1 PEH may be present in a number of conditions characterized by prolonged inflammation and/or chronic infection, as well as in association with many cutaneous neoplasms. Herein, we present a case looking like inflammatory, infectious, and neoplastic skin diseases, in which florid epidermal hyperplasia is a prominent histopathologic feature, and helped in definite diagnosis of benign condition PEH, then a systematic approach in the interpretation of PEH.
Case Report
A 70 year multiparous woman presented to out patient department with lesions on genitalia since 6 months which started as a small lesion but started spreading all over the external genitalia. She is non diabetic and there was no history of bleeds to touch or pain or significant itching. There was also no history of fatigue, loss of weight, apetite, or any bowel / bladder symptoms. On examination she had extensive involvement of vulva and vagina with multiple lesions spreading all over vagina, well – defined, pain less, non foul smelling, no signs of bleeds to touch. There was no involvement of urethra or anus. On per vaginal examination, uterine size and fornices could not be made out due to lesion occupying vulva.
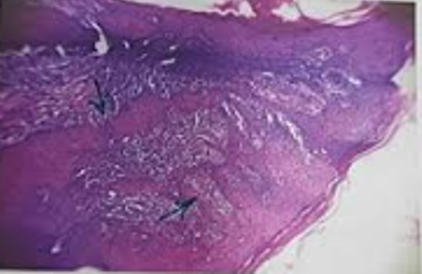
Differential diagnosis thought of were lichen sclerosus, squamous cell carcinoma or vulval cancer. She was advised biopsy and on histopathology a benign lesion of pseudoepitheliomatous hypersplasia was confirmed as depicted in Figure 1.
Discussion
PEH clinically presents as a well-demarcated plaque or nodule with variable degrees of scaling and crusting. The exuberant epithelial hyperplasia corresponds to the ‘‘vegetative’’ or verrucoid nature often noted.1 Ulceration may be present.
Papules or nodules may range from less than 1 cm, for example, in association with granular cell tumor, to several centimeters in diameter, as seen in halogenoderma and deep fungal infections. Lesionswith PEH are usually skin colored or tan pink. However, they may be pigmented when overlying melanoma.2 An adjacent ulcer, burn scar, or colostomy may be present. Occasionally, PEH may present as a large plaque with central scarring and/or an active serpiginous border, commonly described in association with blastomycosis. Lesions containing PEH may increase in size or spontaneously regress. PEH may also arise as an overgrowth in association with a previously diagnosed chronic infection or chronic inflammatory condition. A palpable dermal nodule in association with PEH should raise the possibility of an underlying pathologic process, such as lymphoma or carcinoma. In these cases, a biopsy including the dermis can confirm the diagnosis.1
We are presenting this case report as this diagnosis is encountered infrequently in our clinical practice especially while diagnosing vulvar lesions. In order to differentiate the benign and malignant lesions the biopsy is the gold standard procedure.
PEH is distinguished from SCC by its lack of atypia, confinement to the abnormal collagen, and limited growth. The pathologist must be careful about making a diagnosis of PEH with epidermal thickening, looking carefully for basal atypia and other features of differentiated VIN in the overlying epidermis or dermal proliferation. 3
Local excision of lesion with reconstruction of the tissues involved with multidisciplinary approach is the treatment.
Conclusion
Genital lesions of women with infective or inflammatory or benign or carcinomatous pathology has to be confirmed by multidisciplinary involvement of clinician along with pathologist, surgeon, infectious disease specialists can improvise diagnosis. It will surely impact on better treatment and care for the patient.