Introduction
Weathers and Callihan had first described giant cell fibroma as a separate unique entity among 2000 hyper plastic lesions in the 1970s. It was segregated from the conventional fibroma all because of its distinct histopathological appearance. 2% to 5% of all oral fibrous proliferations are constituted by Giant cell fibroma. This fibrotic soft tissue lesion is said to have an unknown etiology however some reports link its occurrence to viral agents.1 Even minor trauma is considered as an etiological factor due to change in fibroblasts functional status. Giant cell fibroma affects the mandibular gingiva twice more commonly than maxillary gingiva and has an inclination to affect females more. It is named Giant Cell Fibroma due to its characteristic presence of stellate fibroblasts with mutinucleated giant cells on histopathological examination. This sessile or pedunculated lesion is seen more commonly in the young.1, 2 In this paper we present a case of giant cell fibroma in a 30 year old male, and its diagnosis was further confirmed on histopathological examination.
Case Report
A 30 year old male reported to the Department of Oral Medicine and Radiology with a chief complaint of swelling in the lower front tooth region. The patient gave a history of paan chewing habit from the last 7-8 years and consumed it 4-5 times a day. The growth had asymptomatically progressed to its present size. On intraoral examination a swelling was found in the lower labial mucosal region in relation to 42 and 43 which was persistent from the last 2 months. The size of the lesion was approximately 1.5 cm anteroposterioly to 1-1.5 cm mediolaterally in diameter, it was reddish pink in colour obliterating the labial vestibular region. It extended from the attached gingiva region superiorly In relation to 42 and 43 involving the mucogingival region and beyond 2-4 mm inferiorly, extending from the distal attached gingiva in relation to 41 medially to the distal attached gingiva in realtion to 43 laterally. On palpation the surface of the lesion was smooth, fibrosed, non-tender, non scrapable suggestive of provisionally diagnosing it as giant cell fibroma.
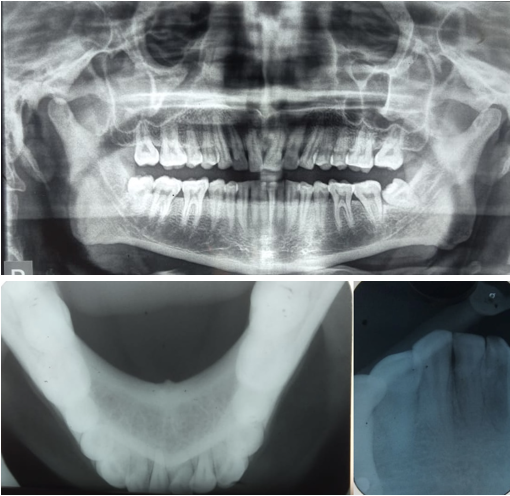
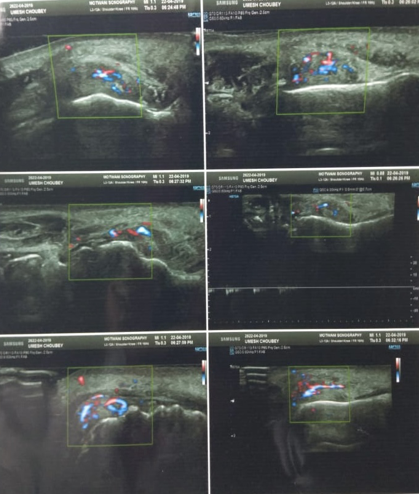
We made a differential diagnosis of Periperal ossifying fibroma, haemangioma, extravasation mucocele, giant cell epulis, soft tissue fibroma. To narrow down our diagnosis patient several investigations were performed. Patient was advised orthopantomogram, occlusal radiograph in relation to mandible and IOPAR in relation to 42 and 43. Radiographic investigations revealed no periapical or periodontal involvement and no calcifications in the region as well. The ultrasonograpy of the soft issue lesion showed a vascular lesion in the vestibule of the mouth with both arterial and venous flow patterns. The patient was advised FNAC and excisional biopsy.
Radiographic investigations
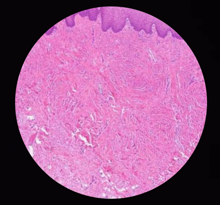
On histopathological examination — H and E staining revealed connective tissue comprised of dense bundles of collagen fibres with a characteristic presence of large spindle shaped stellate and multinucleate giant cells. The overlying epithelium showed features of parakeratinised stratified squamous epithelium.
On FNAC, Smears were studied as haemorrhagic, it showed squamous epithelial cells against a background composed of abundant RBC. The patient was advised various lab investigations including complete blood count, routine blood examination, HIV test, HSV test, HCV test. Patient was negative for HIV HSV, HBV and HCV tests, normal routine blood examination and normal parameters of complete blood count as well.
Final Diagnosis
On excisional biopsy the final diagnosis was confirmed as Giant Cell Fibroma. Patient was recalled after 1 week for suture removal and follow up. Healing of the biopsy site was adequate.
Discussion
This localised reactive proliferation of fibrous connective tissue is a non-neoplastic lesion of oral cavity. Gingival overgrowth and enlargement is a very common feature of gingival disease. Houston in 1982 and Bakos in 1992 commented that it most commonly affects young individuals in the first three decades of life with a female predilection. Its specific cause till date is unknown but according to some reports minor trauma such as brushing or chewing and viral agents are considered as the etiological factors.1, 3 The clinical appearance of this lesion has a tendency to mimic fibroma or papilloma but its distinguished only on histopathological examination. This lesion presents clinically as an elevated small asymptomatic lesion. Regezi et al found that the presence of stellate cells was dependent on the pattern of collagen in the lamina propria and that stellate cells were most often found in oral lesions presenting on the gingival or palate, where the sub mucosa consisted mainly of lamina propria This papillary or bossolated mass with a pebbly surface maybe be pedunculated or sesile usually with a size of less than 1 cm. Its occurrence in the mandibular gingiva is twice more common compared to maxillary gingiva, rarely it may even occur on the buccal mucosa, palate and tongue.3 Rare occurrence of this distinct soft fibrotic lesion has been reported in the extra oral sites like nose, here the lesion appears different histologically by the presence of larger stellate fibroblasts, this shows a tendency to reoccur.4
Histopathological examination are a very important aspect for diagnosis of GCF. It shows a characteristic presence of a number of large stellate and multinucleate giant cells in a loose collagenous stroma. These specific cells are never hyperchromatic. Thus GCF differs from other fibromas, the fibroblasts appear larger and stellate, but they are not hyper chromatic. These lesions have a diffuse, avascular collagen stroma with small and slightly stellate fibroblasts scattered throughout in moderate numbers. Ultrastuctural studies have shown that the multinucleated giant cells and stellate cells are basically unusual fibroblasts.2, 5 GCF is similar to ossifying fibroma clinically, with same hue, but it can be differentiated histologically with the presence of islands of osteogenic cells in ossifying fibroma. GCF and other fibrous hyperplasias like fibromas and fibroepithelial polyps show similar histological features but presence of numerous stellate giant cells differentiates them. The clinical of appearance of GCF having a firm fibroma like mass is because it has an abundance of dense collagen fibres.5
Various immunohistochemical studies have been undertaken to determine the origin of these giant cells. These studies revealed that giant fibroblasts showed negative reactivity for cytokeratin, neurofilament, CD68, HHF, HLA DR, tryptase. The result showed positive staining for vimentin only, thus suggesting a fibroblastic phenotype.3 Desmin showed negative reactivity for giant cells thus ruling out the possibility of a myofibroblastic origin. Studies have even revealed that GCF does not contain elastin but fibroepithelial polyps do contain it. The best treatment modality for GCF is surgical excision in adults and adolescents. However in children it is laser excision or electro surgery. Reoccurrence of GCF is very rare, however some cases of recurrence have been reported. 4, 5
Conclusion
In our routine daily practice we come across various fibrous lesions. These rare lesions should be considered in the differential diagnosis of gingival enlargement. Giant cell fibroma is a unique non neoplastic lesion of oral mucosa which needs. An extensive work up and thorough investigations for its proper diagnosis and treatment planning. 5