- Visibility 199 Views
- Downloads 85 Downloads
- DOI 10.18231/j.sajhp.2024.007
-
CrossMark
- Citation
Acase report on rosuvastatin-induced myopathy
- Author Details:
-
MD Sony
-
Namilikonda Rachana
-
Oragala Sridhar
-
Tejaswi Chillara *
Introduction
Statins (HMG-CoA reductase inhibitors) are the mainstay for treating lipid disorders characterized by low-density lipoprotein cholesterol (LDL-C) elevations. Statins have revolutionized the prevention of primary and secondary coronary atherosclerotic disease due to their lipid-lowering properties and other pleiotropic effects that beneficially affect atherosclerotic plaque stability.[1] A class of disorders known as myopathies results in damage to the muscle fibers and weakening of the muscles. Myopathies come in several forms and can be brought on by autoimmune diseases, genetics, or specific drugs. Muscle cramps, stiffness, and weakness are common symptoms. Depending on the particular form of myopathy, treatment options may include alternative medication, physical therapy, or lifestyle modifications. Most patients very well tolerate statins; however, 10 -12% develop muscle-related adverse effects. [2]
Pathophysiology
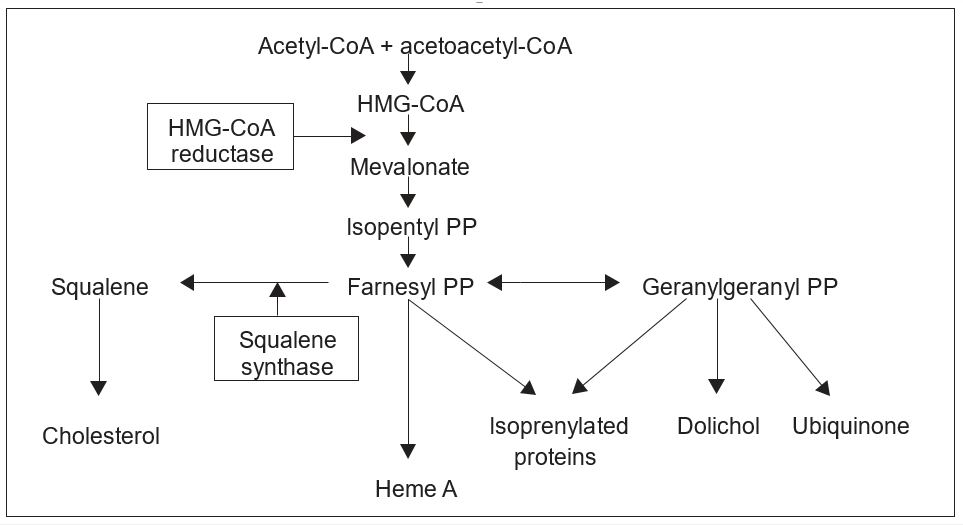
There are several potential explanations for statin-induced myopathy, but the precise mechanism is yet unknown. Leading suggestions include depletion of isoprenoids, suppression of ubiquinone or coenzyme Q10 (CoQ10) synthesis, modification or decrease of cholesterol in the sarcolemal membrane, disruption of calcium metabolism, or autoimmune events.
Depletion of isoprenoid
One proposed mechanism of skeletal muscle cell death is statin-induced isoprenoid deficiency. Isoprenoids are lipids by-products of the HMG-CoA reductase pathway.[5] Farnesyl pyrophosphate (F-PP) and geranylgeranyl pyrophosphate (GG-PP) are the most important isoprenoids in the HMG-CoA reductase pathway (Figure 1). [8] Protein prenylation is the process by which isoprenoids bind to proteins via either farnesylation or geranylgeranylation. Statins reduce the phrenylation of proteins.[6] The reduction of protein prenylation (farnesylation or geranylgeranylation) is thought to increase systolic calcium which activates caspase-3 and leads to cell death. Supporting the role of isoprenoids in statin myopathy is the finding that statin-induced apoptosis in vascular smooth muscle cells is prevented by supplementation with isoprenoids including F-PP and GG-PP.[7], [9]
Ubiquinone inhibition or CoQ10
Ubiquinone or CoQ10 is a constituent of oxidative phosphorylation and ATP production in the mitochondria.[10] Statins inhibit the synthesis of mevalonate, a precursor of CoQ10. Theoretically, statins can cause myopathy by inhibiting the synthesis of CoQ10 in the mitochondria which might compromise the function of the mitochondrial respiratory chain, impair energy production, and ultimately induce myopathy.[10]
Lower sarcolemmal cholesterol levels
Reduced cholesterol levels cause alterations in myocyte membrane cholesterol.[11] Sarcolemal cholesterol deficiency, as a result of the dynamic equilibrium between membrane and plasma lipids, may adversely modify membrane physical properties, such as membrane integrity and fluidity, thus resulting in membrane destabilization. [12] However, two key findings argue against this mechanism. The first is that myotoxicity does not occur in vitro when cholesterol is lowered by inhibiting squalene synthetase in human skeletal myotubules.[13] The second finding is that inherited disorders of the distal cholesterol synthetic pathway result in reduced cholesterol levels without associated clinical myopathy.[14]
Disturbed calcium homeostasis
The regulation of calcium (Ca2+) release and uptake is critical for the normal function of muscle cells.[8] L-type calcium channels mediate the initial increase of intracellular calcium. The sarcoplasmic reticulum's ryanodine receptors are opened by this rise in intracellular Calcium, which results in a significant rise in intracellular Calcium that starts muscle contraction. In a study by Mohaupt et al., muscle biopsies from statin myopathy patients revealed elevated expression of ryanodine receptors 3 (RR3). It is unknown whether elevated RR3 causes or contributes to statin myopathy susceptibility.[4]
Diagnosis
The NLA does not recommend routine measurement of CPK for all patients before starting statin therapy.[3] However, serum creatinine kinase (CPK) can be advised to patients who are presenting with muscle toxicity. Normal levels of CPK are 55-170 U/L in male,30-145 U/L in females.
Treatment
Non-statin lipid-lowering drugs such as ezetimibe, colesevelam, pravastatin, fluvastatin, bempedoic acid, pravastatin, PCSK9 inhibitors like inj. Alirocumab, inj. Evolocumab Alternate statins like atorvastatin, Pravastatin, fluvastatin, Pitavastatin will cause less myopathy.
Case Presentation
History of present illness
A 35-year-old male patient came to the hospital with chief complaints of severe muscle cramps at midnight for 3 years on and off symptoms increased since 3 days. These symptoms are developed after the usage of rosuvastatin. He is a known case of hypertension since 5yrs on regular medication cilnidipine, CAD since 3 years on regular medication rosuvastatin and clopidogrel. He came for a regular checkup at cardiology. The doctor advised atorvastatin instead of rosuvastatin.
Social history
He is married and has 2 sons. He is a financier.
Allergies
No known foods, medicines, or environmental allergies.
Past medical history
He had Hypertension since 5 years
CAD since 3 years
Surgical history
He has no previous surgical history.
Medication history
Tab. cilnidipine 10mg
Tab. rosuvastatin 20mg
Tab. clopitab 75mg
Birth history
The patient was the first child and he had normal weight.
Immunization as per schedule.
Family history
His family history was nill and his brother also suffering with myopathy after using rosuvastatin.
Vitals
General examination
He is cooperative coherent and conscious.
Vitals
Temp: 98.6F
Blood pressure: 130/90mmhg
Pulse rate: 80/min
Respiratory rate: 22/min
SPO 2:98%
Systemic Examination
Respiratory function
NVBS, bilateral air entry present, no additional sound heard.
He has a normal respiratory rate that is 22/min.
Gastrointestinal
Per abdomen soft, no tender, no organomegaly noted.
Cardiovascular
S1 S2 normal
No murmurs heard
Investigations
CBP: HB-13gms%
WBC-8000c/cmm
PLT-2 lakhs
PCV-40%
CPK mm: 1000 mcg/lit after 2 month atorvastatin 190 mcg/lit
Lipid Profile: T. CHOLESTEROL- 220mg/dl
TRIGLYCERIDES-170mg/dl
LDL-179mg/dl
HDL-60mg/dl
ECG: LVH strain noted.
2-D Echo: Inferiorwall hypokinetic
Grade I diastolic dysfunction
Discussion
Statins continue to be the mainstay of the dyslipidemia treatment regimen and a crucial medication for both primary and secondary cardiovascular disease prevention. Doctors can lower the prevalence of statin myopathy by treating each patient differently. A low-dose statin or a statin substation should be administered to patients who have risk factors for statin myopathy, and the dosage should be gradually increased for patients with myopathy, several strategies have been proposed as an alternative to daily statin therapy. Among them are long-acting statins like atorvastatin.
Conclusion
Rosuvastatin is the most commonly used lipid-lowering agent for CAD patients considering its efficacy. A rare side effect of rosuvastatin is myopathy. Replacing with other statins which have less myopathy like atorvastatin and other lipid lowering agents will reduce the myopathy.
Source of Funding
None.
Conflict of Interest
None.
References
- YS Chatzizisis, JM Beigel. Attenuation of inflammation and expansive remodeling by valsartan alone or in combination with simvastatin in high-risk coronary atherosclerotic plaques. Atherosclerosis 2009. [Google Scholar]
- E Bruckert, G Hayem, S Dejager. Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients----the PRIMO study. Cardiovasc Drugs Ther 2005. [Google Scholar]
- JM Mckenney, MH Davidson, TA Jacobson, JR Guyton. Final conclusions and recommendations of the national lipid association statin safety assessment task force. Am J Cardiol 2006. [Google Scholar]
- MG Mohaupt, RH Karas, EB Babiychuk. Association between statin-associated myopathy and skeletal muscle damage. CMAJ 2009. [Google Scholar]
- A Dirks, K Jones. Statin-induced apoptosis and skeletal myopathy. Am J Physiol Cell Physiol 2006. [Google Scholar]
- C Vaklavas, YS Chatzizisis, A Ziakas. Molecular basis of statin-associated myopathy. Atherosclerosis 2009. [Google Scholar]
- CR Harper, TA Jacobson. The broad spectrum of statin myopathy: from myalgia to rhabdomyolysis. Curr Opin Lipidol 2007. [Google Scholar]
- T Abd. Statin-induced myopathy: a review and update. Expert Opin Drug Saf 2011. [Google Scholar]
- C Guijarro, LB Colio, M Ortego. 3-Hydroxy-3-methylglutaryl coenzyme a reductase and isoprenylation inhibitors induce apoptosis of vascular muscle cells in culture. Circ Res 1998. [Google Scholar]
- L Marcoff, PD Thompson. The role of coenzyme Q10 in statin-associated myopathy: a systematic review. J Am Coll Cardiol 2007. [Google Scholar]
- F Westwood, A Bigley, K Randall. Statin-induced muscle necrosis in the rat: distribution, development, and fiber selectivity. Toxicol Pathol 2005. [Google Scholar]
- I Morita, I Sato, L Ma, S Murota. Enhancement of membrane fluidity in cholesterol-poor endothelial cells pre-treated with simvastatin. Endothelium 1997. [Google Scholar]
- T Nishimoto, R Tozawa, Y Amano. Comparing myotoxic effects of squalene synthase inhibitor, T-91485, and 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors in human myocytes. Biochem Pharmacol 2003. [Google Scholar]
- S Baker. Molecular clues into the pathogenesis of statin-mediated muscle toxicity. Muscle Nerve 2005. [Google Scholar]
- Introduction
- Pathophysiology
- Depletion of isoprenoid
- Ubiquinone inhibition or CoQ10
- Lower sarcolemmal cholesterol levels
- Disturbed calcium homeostasis
- Diagnosis
- Treatment
- Case Presentation
- History of present illness
- Social history
- Allergies
- Past medical history
- Surgical history
- Medication history
- Birth history
- Family history
- Vitals
- Systemic Examination
- Discussion
- Conclusion
- Source of Funding
- Conflict of Interest
How to Cite This Article
Vancouver
Sony M, Rachana N, Sridhar O, Chillara T. Acase report on rosuvastatin-induced myopathy [Internet]. South Asian J Health Prof. 2024 [cited 2025 Sep 12];7(1):28-31. Available from: https://doi.org/10.18231/j.sajhp.2024.007
APA
Sony, M., Rachana, N., Sridhar, O., Chillara, T. (2024). Acase report on rosuvastatin-induced myopathy. South Asian J Health Prof, 7(1), 28-31. https://doi.org/10.18231/j.sajhp.2024.007
MLA
Sony, MD, Rachana, Namilikonda, Sridhar, Oragala, Chillara, Tejaswi. "Acase report on rosuvastatin-induced myopathy." South Asian J Health Prof, vol. 7, no. 1, 2024, pp. 28-31. https://doi.org/10.18231/j.sajhp.2024.007
Chicago
Sony, M., Rachana, N., Sridhar, O., Chillara, T.. "Acase report on rosuvastatin-induced myopathy." South Asian J Health Prof 7, no. 1 (2024): 28-31. https://doi.org/10.18231/j.sajhp.2024.007
